Impact
Publications:
- Use of telehealth for health care of Indigenous peoples with chronic conditions: a systematic review. Read more...
Fraser, S, Mackean, T, Grant, J, Hunter, K, Towers, K and Ivers | Rural and Remote Health 2017 - Burns injury models of care: a review of quality and cultural safety for care of Indigenous children. Read more...
Fraser, S, Grant, J Mackean, T, Hunter, K, Holland, AJA, Clapham, K, Teague, WJ and Ivers | Burns - What informs care? Descriptions by multidisciplinary teams about burns care for Aboriginal and Torres Strait Islander children. Read more...
Fraser, S, Grant, J, Mackean, T, Hunter, K, Keeler, N, Clapham, K, Teague, WJ, Potokar, T and Ivers | Burns - Walking together to create harmony in research: A Murri woman’s approach to Indigenous research methodology. Qualitative Research in Organizations and Management. Read more...
Coombes J, Ryder C. | Qualitative Research in Organizations and Management - Factors that impact access to ongoing health care for First Nation children with a chronic condition. Read more...
Coombes J, Hunter K, Mackean T, Holland AJ, Sullivan E, Ivers R | BMC Health Services Research - A Understanding burn injuries in Aboriginal and Torres Strait Islander children: protocol for a prospective cohort study. Read more...
Ivers, RQ., Hunter, K., Clapham, K., Coombes, J., Fraser, S., Lo, S., Gabbe, B., Hendrie, D., Read, D., Kimble, R., Quinn, L., Towers, K., Potokar, T., Mackean, T., Grant, J., Lyons, RA., Jones, L., Eades, Daniels, J, Holland J | BMJ Open
- Equity in functional and health related quality of life outcomes following injury in children - a systematic review. Read more...
Ryder, C., Mackean, T., Hunter, K., Williams, H., Clapham, K., Holland, A. J. A., & Ivers, R. | Critical Public Health - Indigenous research methodology – weaving a research interface. Read more...
Ryder, C., Mackean, T., Coombs, J., Williams, H., Hunter, K., Holland, A. J. A., & Ivers, | International Journal of Social Research Methodology - Efficacy and cultural appropriateness of psychosocial interventions for Aboriginal and Torres Strait Islander paediatric burn patients and caregivers: a systematic review. Read more...
Williams H., Hunter K., Clapham K., Kimble R., Griffin B | BMC Public Health - The Journey of Aftercare for Australia’s First Nations Families Whose Child Had Sustained a Burn Injury. Read more...
Coombes J, Hunter K, Mackean T, Sullivan E, Ivers R. | BMC Health Services Research - Burn Injuries in Hospitalised Australian Children - An Epidemiological Profile. Read more...
Ryder, C. Mackean, M. Hunter, K. Rogers, K. Holland, J. Ivers, R - Factors Contributing to Longer Length of Stay in Aboriginal and Torres Strait Islander Children Hospitalised for Burn Injury. Read more...
Ryder, C. Mackean, M. Hunter, Towers, K. K. Rogers, K. Holland, J. Ivers, R - Yarning up about out-of-pocket healthcare expenditure in burns with Aboriginal families. Australian and New Zealand Journal of Public Health. 2021. Read more...
Ryder, C, Mackean, T. Hunter, K. Coombes, J. Holland, A. Ivers, R. - “They Are Worth Their Weight in Gold”: Families and Clinicians’ Perspectives on the Role of First Nations Health Workers in Paediatric Burn Care in Australia. Read more...
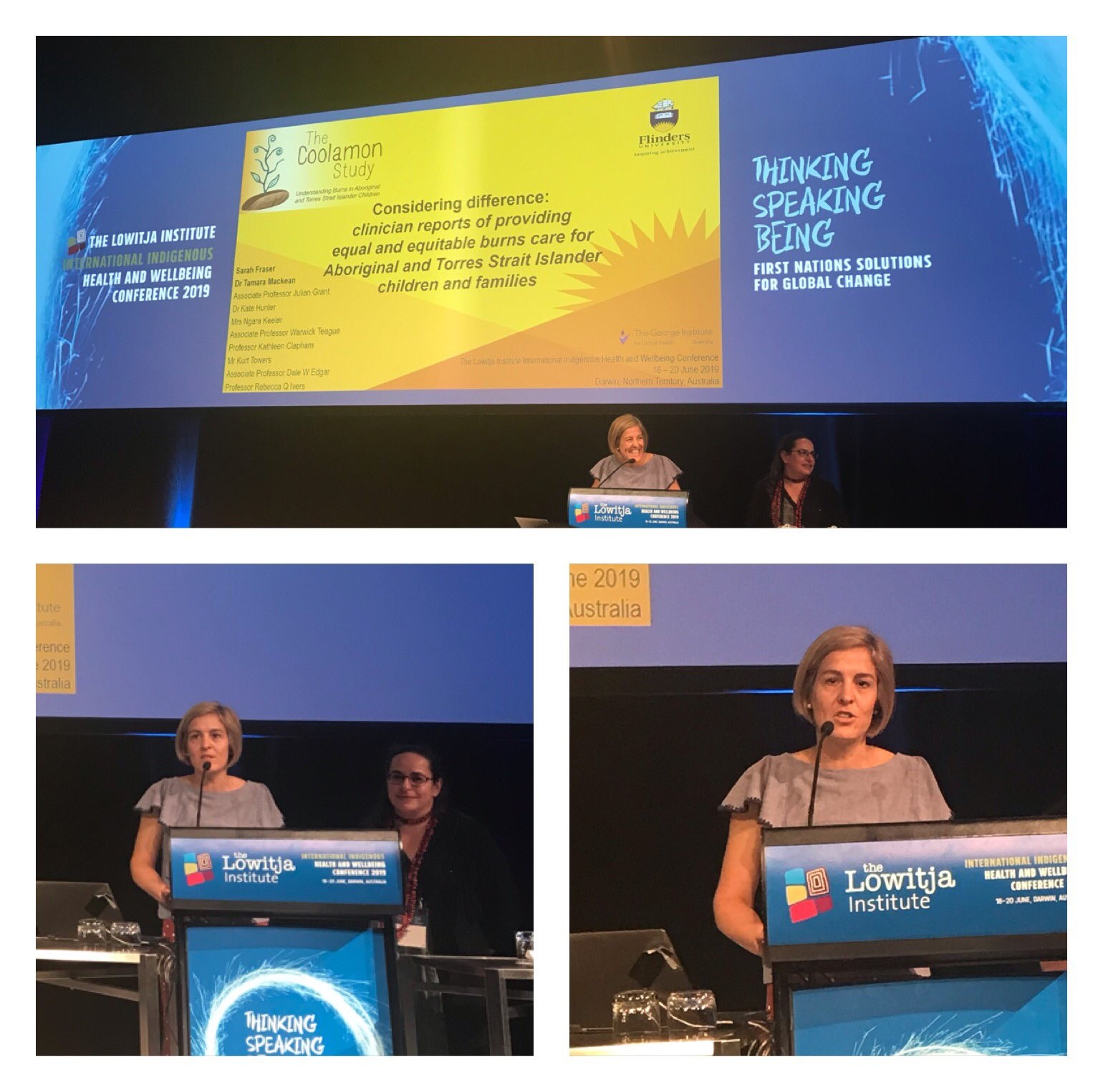
Julieann Coombes, Sarah Fraser, Kate Hunter, Rebecca Ivers, Andrew Holland, Julian Grant, and Tamara Mackean.Int J Environ Res Public Health. 2021 Mar; 18(5): 2297. - Considering difference: clinician reports insights into providing equal and equitable burns care for Aboriginal and Torres Strait Islander children and families. Read more...
Sarah Fraser, Julian Grant, Tamara Mackean, Kate Hunter, Dale Edgar, Kurt Towers, Warwick Teague and Rebecca Ivers.
Presentations
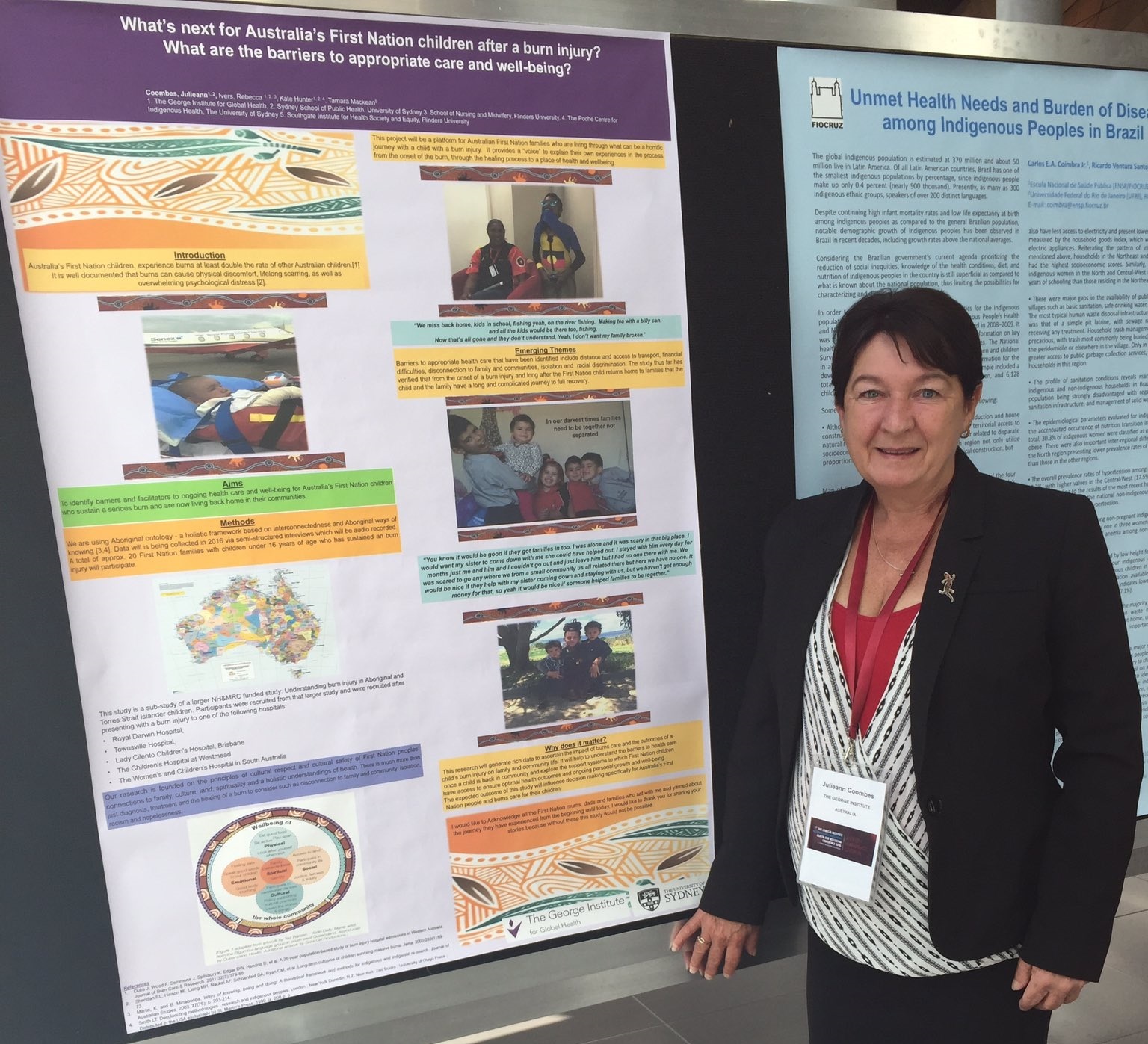
Australia’s First Nation Children’s need for Culturally Appropriate Burn After Care. Download here...
Burden of Burns in Australian Children. Download here...
The Coolamon study. Download here...
Burn injury models of care: a review of quality and cultural safety for care of Indigenous children. Download here...
What informs care? Descriptions by multidisciplinary teams about burns care for Aboriginal and Torres Strait Islander children and families. Download here...
Considering difference:
clinician reports of providing
equal and equitable burns care for Aboriginal and Torres Strait Islander children and families. Download here...